Thank you for Subscribing to Healthcare Business Review Weekly Brief
Be first to read the latest tech news, Industry Leader's Insights, and CIO interviews of medium and large enterprises exclusively from Healthcare Business Review
Best Practices for Safe and Effective Medical Sterilization
Effective medical sterilization involves understanding methods, maintaining equipment, and managing resources. Healthcare facilities ensure a secure environment by prioritizing education and quality assurance.
By
Healthcare Business Review | Thursday, June 26, 2025
Stay ahead of the industry with exclusive feature stories on the top companies, expert insights and the latest news delivered straight to your inbox. Subscribe today.
Fremont, CA: In the healthcare sector, medical sterilization is essential to ensure that the instruments and devices used in patient care are free from harmful microorganisms.Despite its essential role, various challenges can impact efficiency and safety. One of the fundamental challenges in medical sterilization lies in understanding the various methods available and their appropriate applications.
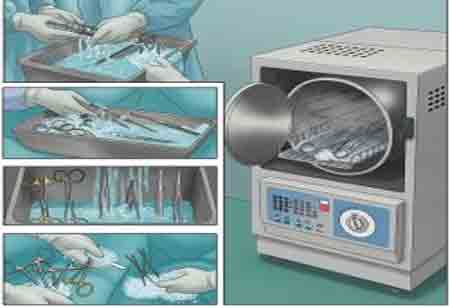
Common sterilization techniques include steam sterilization (autoclaving), ethylene oxide gas (EtO) sterilization, hydrogen peroxide plasma, and radiation sterilization. Each method has distinct advantages and limitations, which can complicate decision-making. For instance, steam sterilization is the most commonly used method due to its efficacy and speed. However, it is unsuitable for all materials, such as those sensitive to heat or moisture.
On the other hand, ethylene oxide is effective for heat-sensitive items but requires lengthy aeration periods to eliminate toxic residues. To navigate these complexities, healthcare facilities must invest in staff training and maintain clear protocols corresponding to different materials' specific requirements. Ongoing education ensures that those responsible for sterilization processes are well-versed in current practices and technologies, enhancing overall efficacy and safety.
Maintaining Equipment and Compliance
Another significant challenge in medical sterilization is maintaining the equipment and ensuring compliance with industry standards. Regular maintenance is essential; failure to do so can lead to equipment malfunction, resulting in ineffective sterilization and increased risk of infection. Facilities must establish a rigorous maintenance schedule and adhere to manufacturer recommendations, which can sometimes be overlooked under the pressures of daily healthcare operations.
In addition, compliance with regulations from organizations like the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) can be daunting. These regulations outline specific standards for sterilization processes, including documentation and monitoring of sterilization cycles. Non-compliance can lead to serious legal ramifications and jeopardize patient safety. Implementing quality assurance programs that include regular audits and checks can help identify areas of improvement and ensure adherence to protocols. Ensuring all staff members know compliance requirements and participate in ongoing training will mitigate these challenges significantly.
Addressing Resource Constraints
Resource constraints present an ongoing challenge in many healthcare facilities, particularly in resource-limited settings. Budget restrictions can affect the purchase of high-quality sterilization equipment or the recruitment of skilled personnel, leading to suboptimal practices. In such environments, improvisation often becomes necessary, which can compromise sterility and increase the risk of healthcare-associated infections.
To address these constraints, healthcare facilities must prioritize strategic resource allocation. This involves identifying key investment areas and exploring alternative funding sources, such as grants or partnerships. Moreover, facilities can explore cost-effective sterilization alternatives, like repurposing existing equipment or utilizing community resources for training and support. Collaborating with neighboring facilities or institutions for shared services can mitigate costs and improve access to best practices.





