Thank you for Subscribing to Healthcare Business Review Weekly Brief
Be first to read the latest tech news, Industry Leader's Insights, and CIO interviews of medium and large enterprises exclusively from Healthcare Business Review
The Business of Healthcare in Understanding Cost Structures and Profit Models
The healthcare industry is a cornerstone of modern society, blending medical innovations and quality care delivery with business practices required to sustain its operations.

By
Healthcare Business Review | Monday, February 24, 2025
Stay ahead of the industry with exclusive feature stories on the top companies, expert insights and the latest news delivered straight to your inbox. Subscribe today.
Healthcare cost structures and profit models play a crucial role in shaping the financial sustainability of medical institutions.
FREMONT, CA: The healthcare industry is a cornerstone of modern society, blending medical innovations and quality care delivery with business practices required to sustain its operations. To understand the healthcare business, it's essential to explore its cost structures and profit models, which, while complex, are designed to balance patient care and commercial viability.
Key Cost Structures in Healthcare
Operational expenses form a substantial portion of healthcare expenditures, encompassing staff salaries, facility maintenance, and technology utilization. Compensation for healthcare professionals—including doctors, nurses, technicians, and administrative staff—constitutes a significant financial commitment. Additionally, hospitals and clinics require continuous upkeep, covering utilities, sanitation, and infrastructure maintenance. Integrating medical technology, such as diagnostic tools, imaging equipment, and electronic health records, further adds to recurring costs.
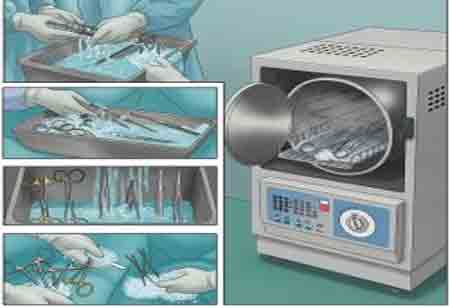
Beyond operational expenses, healthcare systems must allocate significant funds for supplies and equipment. Surgical instruments, disposable medical materials, and personal protective equipment (PPE) are essential for daily operations. At the same time, advanced machinery like MRI scanners represents a high initial investment and ongoing maintenance costs.
Training and compliance expenditures are another critical consideration, ensuring that healthcare professionals receive continuous education to meet evolving regulatory and legal standards. Regular audits and adherence to health and safety guidelines contribute to these costs.
Furthermore, research and development (R&D) investments drive medical innovation, particularly in pharmaceuticals and medical technology. While costly, these advancements enhance treatment options, improve patient outcomes, and contribute to the long-term evolution of healthcare.
Profit Models in Healthcare
Healthcare institutions operate under various revenue-generating models. The traditional fee-for-service (FFS) model charges patients for individual procedures, consultations, and diagnostic tests, often incentivizing volume over quality of care. In contrast, value-based care (VBC) emphasizes patient outcomes, rewarding providers for efficiency, cost-effectiveness, and quality metrics rather than service volume.
Insurance-based models, where private insurers or government programs act as intermediaries, reimburse healthcare providers at pre-negotiated rates. These arrangements significantly influence provider revenue streams. Meanwhile, direct-to-consumer models, including telemedicine and concierge healthcare, bypass traditional insurance frameworks, offering patients predictable pricing through subscription-based or flat-fee structures.
The healthcare sector is evolving into a tightly integrated ecosystem, blending service providers, insurers, and tech platforms. With ongoing technological advances and societal demands for better accessibility, healthcare models need continuous innovation. Success will hinge on providers' abilities to align patient welfare with sustainable business practices.
The healthcare industry is undergoing significant transformation, driven by technological advancements, evolving patient expectations, and a growing emphasis on equity. One key trend is the integration of digital health solutions, with telehealth and digital tools enhancing operational efficiency, reducing costs, and improving accessibility for patients. Simultaneously, healthcare businesses prioritize health equity initiatives by addressing social determinants of health, ensuring that services are inclusive and accessible to diverse populations. Adopting artificial intelligence and automation is another pivotal shift, with AI-powered tools streamlining diagnostics, workflow management, and predictive analytics. While these technologies enhance efficiency, they require substantial initial investment. Additionally, mergers and acquisitions reshape the competitive landscape, enabling providers to achieve economies of scale, optimize costs, and expand their market presence. Together, these trends reflect a healthcare ecosystem that is increasingly data-driven, patient-centric, and strategically consolidated.
Understanding healthcare cost structures and profit models is crucial for stakeholders navigating this multifaceted industry. As pressures on the system grow, the delicate balance between maintaining affordability and achieving financial sustainability must be a priority for policymakers, business leaders, and healthcare providers.