Thank you for Subscribing to Healthcare Business Review Weekly Brief
Be first to read the latest tech news, Industry Leader's Insights, and CIO interviews of medium and large enterprises exclusively from Healthcare Business Review
Transitioning from Fee-for-Service to Value-Based Care Models
The healthcare landscape is transforming significantly, shifting from the traditional fee-for-service (FFS) model to value-based care (VBC) models.
By
Healthcare Business Review | Friday, January 17, 2025
Stay ahead of the industry with exclusive feature stories on the top companies, expert insights and the latest news delivered straight to your inbox. Subscribe today.
By redefining traditional care delivery, VBC models are paving the way for more effective, equitable, and sustainable healthcare systems, making them a critical focus in the evolution of modern medicine.
FREMONT, CA: The healthcare landscape is transforming significantly, shifting from the traditional fee-for-service (FFS) model to value-based care (VBC) models. This shift prioritizes patient outcomes and quality of care over the volume of services provided.
Value-Based Care (VBC) models mark a transformative shift in healthcare delivery by prioritizing the value and quality of care provided rather than the service volume. These models are designed to improve patient health outcomes while reducing costs, creating a win-win scenario for patients and providers. By aligning provider incentives with patient-centered goals, VBC models encourage healthcare systems to focus on delivering high-quality care, enhancing patient satisfaction, and optimizing resource use.
A cornerstone of VBC models is their emphasis on delivering high-quality care. Providers are incentivized to achieve better patient health outcomes through evidence-based practices and continuous quality improvements. Enhancing patient satisfaction is another critical objective, with patient experience metrics often integrated into performance evaluations. Additionally, VBC models aim to reduce healthcare costs by prioritizing preventative care and eliminating unnecessary procedures, fostering a more sustainable healthcare ecosystem.
Several key components define the VBC approach. Patient-centered care lies at its heart, emphasizing the importance of engaging patients in healthcare decisions through shared decision-making. Strong care coordination is equally crucial, requiring seamless collaboration among primary care physicians, specialists, and hospitals to ensure cohesive and efficient treatment pathways. Data analytics play a vital role in tracking patient outcomes and identifying areas for improvement. At the same time, technologies such as electronic health records (EHRs) and telemedicine are indispensable tools that enable streamlined care delivery.
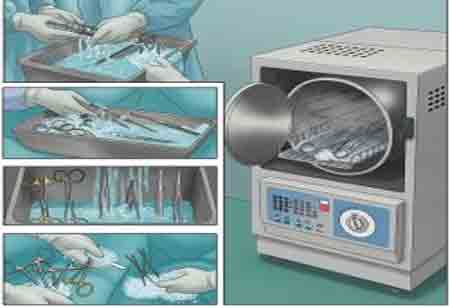
VBC models manifest in various forms to suit different healthcare contexts. Pay-for-performance models reward providers for achieving specific quality and cost benchmarks, fostering accountability and excellence. Bundled payments allocate a fixed amount for a defined episode of care, such as a surgical procedure, encouraging cost-efficient care management. Capitation models, where providers receive a set monthly payment per patient regardless of the services provided, further incentivize resource optimization and preventive care initiatives.
The benefits of adopting VBC models are far-reaching. Patients experience improved health outcomes due to a heightened focus on quality and preventative care. The healthcare system benefits from reduced costs as unnecessary procedures are minimized and resources are utilized more efficiently. Furthermore, emphasizing patient-centered care enhances patient satisfaction, fostering trust and confidence in the healthcare system.
The transition from FFS to VBC models is a complex process, but it is essential for improving the quality and affordability of healthcare. VBC models can help create a more sustainable healthcare system by focusing on patient outcomes and reducing costs.