Thank you for Subscribing to Healthcare Business Review Weekly Brief
Be first to read the latest tech news, Industry Leader's Insights, and CIO interviews of medium and large enterprises exclusively from Healthcare Business Review
Trends in Medical Equipment Sterilization Across APAC
Sterilization in healthcare is advancing with low-temperature method, radiation technique and AI-driven system. These innovation enhance efficiency support sustainability, and ensure safer, more adaptable sterilization across various medical setting.

By
Healthcare Business Review | Monday, June 09, 2025
Stay ahead of the industry with exclusive feature stories on the top companies, expert insights and the latest news delivered straight to your inbox. Subscribe today.
Fremont, CA: Sterilization techniques are evolving to meet the growing demands of modern healthcare. Traditional methods remain valuable, but advancements are introducing faster, safer, and more versatile solutions. From low-temperature systems to AI integration, emerging technologies enhance efficiency, support sustainability, and reshape how sterilization is performed across diverse medical settings.
Advancements in Sterilization Techniques
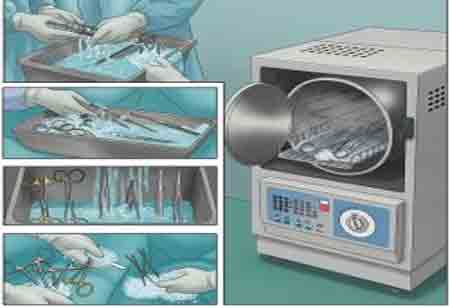
Traditional sterilization methods like steam autoclaving and dry heat have been industry standards for decades. While they remain widely used due to their reliability, newer techniques have emerged to address limitations in material compatibility and processing time. Low-temperature sterilization processes, such as hydrogen peroxide gas plasma and vaporized peracetic acid, have gained traction for sterilizing heat-sensitive medical instruments without compromising their integrity. These methods offer shorter cycle times and are generally more compatible with modern devices made of plastic and composite materials.
Another growing trend involves advanced radiation-based methods, including electron beam and gamma irradiation. These techniques are especially prevalent in sterilizing pre-packaged single-use items. Though initially limited by equipment costs and safety concerns, improvements in system design and safety protocols have made them more accessible and scalable. Healthcare facilities and manufacturers in APAC have increasingly adopted these methods for their precision and consistency.
The demand for flexible sterilization options has also encouraged the development of portable and decentralized sterilization units. These compact systems are especially beneficial in remote settings or temporary medical facilities where traditional infrastructure may be lacking. Sterilizing instruments on-site reduces reliance on central processing units and enhances the speed of medical response in critical environments.
Sustainability and Regulatory Influence
Growing environmental awareness within the healthcare industry has significantly influenced sterilization practices. Chemical sterilants and traditional energy-intensive methods are being scrutinized for their environmental impact. In response, there is a shift toward eco-friendlier sterilization alternatives that reduce emissions, minimize waste, and conserve energy. Innovations include sterilization systems that use fewer toxic chemicals or recycle gases in closed-loop processes to reduce atmospheric release.
Regulatory guidelines continue to play a central role in shaping sterilization trends. Authorities have raised standards for efficacy, traceability, and validation, compelling healthcare providers to implement more rigorous monitoring and documentation practices. This has led to greater adoption of digital sterilization tracking systems, which help maintain compliance and accountability. Data-driven sterilization workflows improve process transparency and enable better decision-making.
Integrating artificial intelligence and smart sensors also influences the sterilization process. These technologies monitor sterilization parameters in real-time, detect anomalies, and adjust conditions to optimize outcomes. The result is improved consistency, reduced risk of human error, and better resource utilization.